The concept of constructing movement system diagnoses is an initiative through the Academy of Neurologic Physical Therapy. The goal is to standardize physical therapy neurological diagnosis through consistent and evidence-based terminology describing problems we identify with the following movement systems: integumentary, neurological, musculoskeletal, cardiovascular, pulmonary, and endocrine. The initiative is targeted to inform our examination, evaluation, diagnosis, prognosis, outcomes, and interventions. Hedman et al. describe the need to see this initiative to fruition by stating, “while this practice may be inherent for many PTs, the profession lacks a consistent approach to movement analysis and, importantly, lacks the terminology to describe movement dysfunction in a standardized manner.”1
In my opinion, this initiative is labeling the optimal goal that PTs and PT educators have worked toward accomplishing since the beginning of our profession. We all want to do the best job at figuring out why our clients have difficulty moving through a detailed exam of the movement system. We want to provide the best treatments and communicate our findings, and plan in the best way possible. However, as our profession and vast skills evolve, we realize that we do not all agree or possess awareness relating to the optimal ways to investigate, describe, and treat these disorders. Some of us simply lack the opportunities to train to gain the necessary skills to provide optimal care.
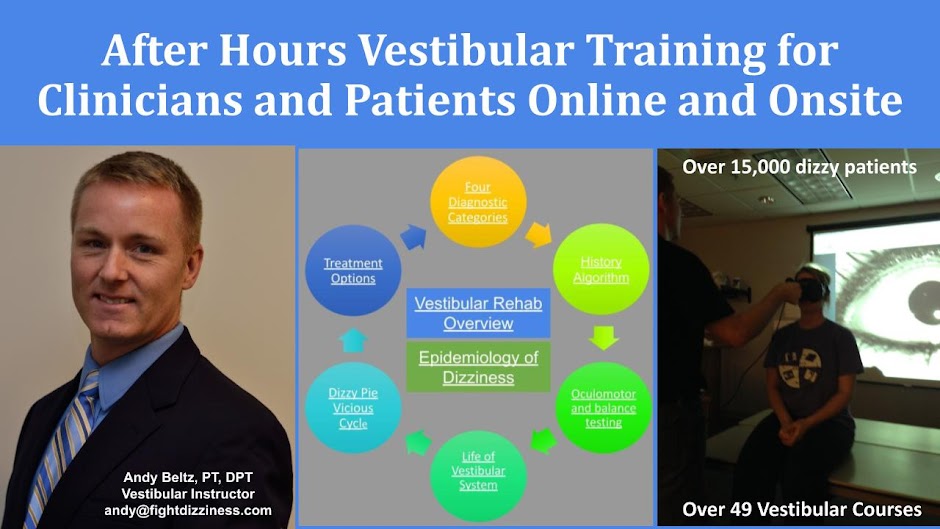
As a neuro/vestibular PT, I have had the opportunity to teach and mentor hundreds of therapists over the last 21 years in evaluating and treating some of the most common disorders that impact our balance system. I have helped train these therapists onsite and through conversations over the phone, email, and texting. I have been able to build long-term relationships with many of these therapists. As a result, I have discovered that unless PTs are seeing a high volume of clients with dizziness and balance disorders, they will become confused when trying to complete an efficient history, objective exam, evaluation, assessment, and treatment.
Even if PTs complete several courses directed at teaching these skills, a high caseload of clients with the appropriate diagnosis is needed consistently so that the skills can be practiced regularly. Intense professional drive is required to put newly learned skills into practice. If PTs do not have a high caseload of clients with the appropriate diagnosis, they will not practice the things they have learned, and concepts learned in courses can quickly be forgotten.
Lack of patients with a key diagnosis that complements a PT's specialized training is crucial. Without these two elements combined at the proper time in the proper environment, providing optimal quality care can be very difficult. For instance, some PTs may forget to ask clients questions relating to the timing or triggers of symptoms. As a result, discovering all reasons for dizziness or balance disorders may not occur. PTs may omit core oculomotor, vestibular, and balance tests in the exam. They may exclude postural or sensory testing. This may lead to unnecessary discomfort for clients trying to overcome their movement disorders. PTs may become confused when a chosen treatment is not as effective as expected, leading to an unnecessary delay in recovery.
In summary, I support an evidence-based standardized approach to examining, evaluating, assessing (including prognosis, predicting outcomes), and providing optimal evidence-based interventions. Building movement system diagnosis tools and databases will help provide guidance for PTs wanting to provide optimal care to all clients. It will provide a framework that will guide decision-making, help build the best skills over larger populations of PTs, and ultimately help more people experience optimal outcomes.
“I attest that this submission represents my own work and is compliant with Arcadia’s standards for academic integrity.”
1. Hedman LD, Quinn L, Gill-Body K, et al. White Paper: Movement System Diagnoses in Neurologic Physical Therapy. J Neurol Phys Ther. 2018;42(2):110-117.