Vestibular
Screening and Treatment in Therapy Practice: When to Refer
Where: Walsh University
When: December 3, 2016- 8:00-4:30
Who: PTs and PTAs
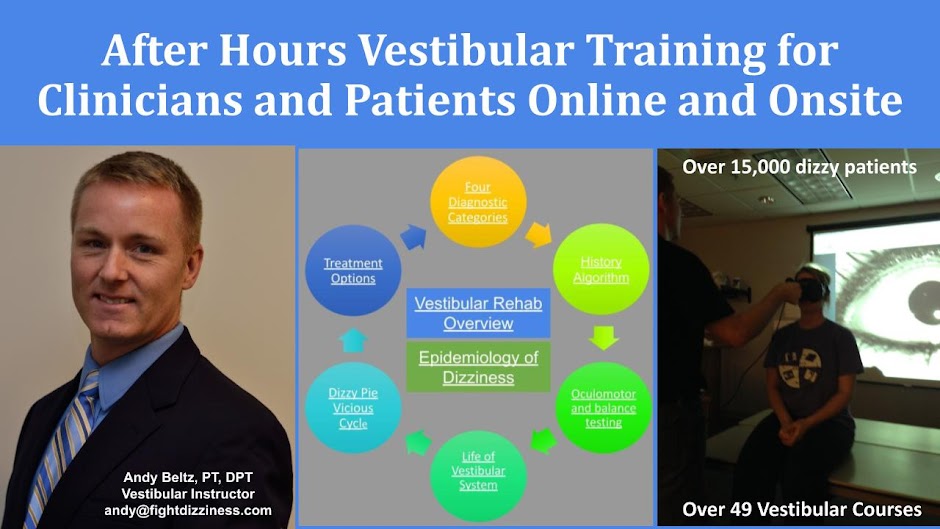
Instructor: Andy Beltz, PT, Vestibular Therapist and Principal Investigator
Skill level: There will be basic, intermediate and advanced concepts
reviewed. This course is ideal for therapists who want to assess and expand
their skills helping clients who are battling dizziness.
Course Description
Vestibular Screening and
Treatment in Rehab Settings: When to Refer is ideal for therapists who want to assess
and expand their skills helping clients who are battling dizziness.
● You are
evaluating a 45-year-old male for headaches, neck pain, and dizziness and he
suddenly develops severe spinning and vomiting. What should you do next?
● A 68-year-old
male has worked with you three visits on improving his balance and has made
minimal progress. Are there any simple
bedside tests that could be done to confirm the presence of a vestibular
dysfunction? Would this individual
benefit from vestibular exercises?
● A 72-year-old female, who is status post two
weeks left total knee arthroplasty, refuses to lie down to perform her
exercises for fear of becoming dizzy. She also becomes very dizzy sitting up. Is there something more you could do to help?
With
over 435 different words and phrases clients have used to describe dizziness,
finding relief can sometimes be frustrating. In addition, therapists may not
always know when to try to help or refer them to a vestibular specialist. These case studies, combined with video
analysis, will be reviewed to build skills relating to screening, evaluation,
and treatment of the most common vestibular disorders. A discussion regarding when to refer clients
to other practitioners will take place.
Course objectives:
Upon
completion of this seminar, the attendee will be able to:
1. List the four
most important goals for the clinician screening a client with dizziness.
2. Define acute vestibular
syndrome (AVS).
3. Name three
bedside tests that, when used together, may be more sensitive than MRI at
identifying an acute posterior stroke.
4. Recognize
necessary clinical skills and tools needed to identify and treat a vestibular
hypofunction.
5. Describe how to
evaluate and treat the most basic form of benign paroxysmal positional vertigo
(BPPV).
6. Compare and
contrast the screening process for orthostatic hypotension (OH) and BPPV.
7. Explain when the
four types of vestibular rehabilitation should be utilized.
8.
Discuss when clients should be referred to vestibular specialty
clinics and other specialists.
Time Schedule With Objectives
Topic
|
Time
|
Vestibular
Rehab Overview:
Upon
completion of this section, the learner will be able to:
● Identify when vestibular
rehab and/or other types of treatment options are needed.
● List the four
most important goals for the clinician screening a client with dizziness.
Dizziness
History:
Upon
completion of this section, the learner will be able to:
● Name key
questions needed to compartmentalize client’s symptoms and guide prediction
of outcomes with vestibular rehab (VR).
● Learn how to
identify individuals who may be likely to vomit during the vestibular
exam/treatment.
● Learn how to
identify the "highly sensitive person" before it's too late.
● Recognize the
importance of understanding the "trap of IT" during the history.
● Discuss the
need to learn each individual’s unique “dizzy language.”
|
8:00-9:00
|
Vestibular
History and Exam:
Upon
completion of this segment the learner will be able to:
● Compare stages
of blizzards and tornadoes with common vestibular disorders and discuss how
timing of testing and treatment impact outcomes.
● Define acute
vestibular syndrome and how it relates to “The Dizzy Pit.”
● Name questions helpful in predicting
those at risk for vertebral artery dissection and/or stroke.
● Name three bedside tests that, when
used together, may be more sensitive than MRI at identifying an acute
posterior stroke.
● List some of
the most common causes of a vestibular hypofunction.
● Recognize
necessary clinical skills and tools needed to identify and treat a vestibular
hypofunction.
● Describe how to
name nystagmus.
● Discuss when
clients should be referred to vestibular specialty clinics and other specialists.
|
9:00-10:00
|
Break
|
10:00-10:15
|
Vestibular
Exam:
Upon
completion of this segment the learner will be able to:
● Name various
stages in which a vertebral artery dissection may present in your setting.
● Discuss and
demonstrate ways to identify stroke through the "HINTS" test
battery.
● Discuss
Horner's sign and it's implications.
● Name tests
helpful for identifying "the highly sensitive person."
● Explain how
Alexander’s law is helpful in predicting outcomes.
|
10:15-11:15
|
Vestibular Exam
and Treatment
● Name and
perform key bedside tests helpful for identifying a vestibular hypofunction.
(Head Impulse, Mastoid Vibration, Dynamic Visual Acuity Test, Spontaneous and
Gaze Hold Nystagmus Tests)
● Discuss and demonstrate
seven key elements helpful when implementing a vestibular rehabilitation
program (treatment options).
● List key
coaching and education elements required to maximize outcomes.
|
11:15-12:15
|
Lunch
|
12:15-1:15
|
Benign
Paroxysmal Positional Vertigo (BPPV) Vs. Orthostatic Hypotension (OH): Going
Beyond, “What do you mean by dizzy?”
●
Describe how to set the most sensitive trap for identifying the
presence of BPPV and/or OH in your clients.
●
Compare and contrast the screening process for OH and BPPV.
|
1:15-2:15
|
BPPV- From
Captivity To Freedom:
● Name and perform key tests helpful for
identifying posterior canal BPPV.
● Name and perform key tests helpful for
identifying lateral canal BPPV. Demonstrate modifications that can be made
for testing individuals with stiff spines.
● Demonstrate ways to confirm presence of
BPPV if history is consistent with BPPV, but no signs exist during exam.
● Describe likelihood for secondary BPPV
in presence of other vestibular disorders.
● Discuss when avoidance should be taught
in treatment of BPPV.
● Recognize how to Identify and treat the
"rebellious" BPPV cases.
● Demonstrate new treatment options for
lateral canal BPPV.
● Discuss when the Brandt Daroff exercise
is indicated.
● Recognize benefits of certain
medications when treating some forms of BPPV.
|
2:15-3:15
|
Break
|
3:15-3:30
|
Vestibular
Rehab Treatment:
Upon
completion of this segment, the learner will be able to:
● Explain when
the four types of vestibular rehabilitation should be utilized.
● Discuss impact
of sympathetic and parasympathetic nervous system imbalance on vestibular
rehab prognosis.
● Describe
techniques available to optimize nervous system health.
● Discuss
modifications needed when planning treatment for the Highly Sensitive Person
and Type A personalities.
● Draw graphs
that assist in recognizing how to plan treatments of clients battling
dizziness
● Discuss impact
of identifying individuals "adaptive reserve" when planning
treatments.
|
3:30-4:30
|
About the Speaker:
Andy Beltz, Physical Therapist, has specialized in helping
thousands of clients battle disorders causing dizziness since May of 2000 at
the Aultman Health Foundation in Canton, Ohio.
Since 2001, he has used infrared lenses (device used to study eye movements
in the dark) and has been a vestibular specialty clinical instructor/capstone
supervisor for 16 PT students in the outpatient setting. He leads a
vestibular rehab observation program that has served over 60 Medical Residents
and has taught continuing education courses on vestibular rehabilitation since
2003. As the principal investigator (ClinicalTrials.gov
Identifier: NCT02626052), he has enrolled over 216 clients in his diagnostic
accuracy study comparing room light and fixation blocked vestibular tests. He
is a mentor for a concussion study being conducted by one of his peers, serves
as chair-elect on Aultman’s Research Council, and is an adjunct faculty member
for Aultman’s Research Academy. He has
passed two of Dr. Susan Herdman’s competency based courses (Vestibular Rehab
and Vestibular Function Test Interpretation and Application to Rehabilitation).
He currently works full time as the therapy lead with a great team of
colleagues at Aultman Tusc Therapy. Mr.
Beltz graduated from Bowling Green State University in consortium with The
Medical College of Ohio (now University of Toledo) with his bachelor’s degree
in physical therapy in 1999. He began working in acute care at Aultman in
November of 1999 and has practiced vestibular rehab in all therapy
settings. He has been a member of
the APTA since 1997.