Red Light Dizziness and Green Light Dizziness
Red Light Pain and Green Light Pain
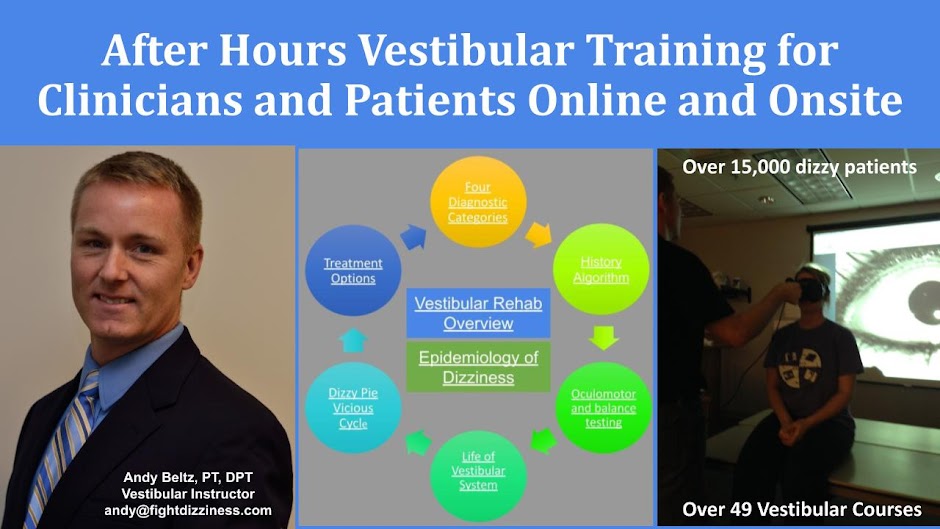
My role as a dizzy therapist is to get rid of the dizziness trigger as quickly as possible. This might mean fixing the BPPV, promoting vestibular adaptation for neuritis, or teaching how to prevent Migraines. These triggers often create intense spinning that require a special kind of treatment. I call this type of spinning: "Red Light Dizziness." When individuals have red light dizziness they need to stop, call me, do a maneuver, take a medication, etc. However, once the red light dizziness is gone, they need to move normally. This leads to how to break the vicious cycle of dizziness. They need to adapt a "bring it on baby" mentality. They welcome dizziness as an opportunity to improve and promote healing. I call this stage "green light dizziness." Green light means go. The feeling that you could become dizzy is not a sign you will become dizzy. I spend a lot of time educating individuals because it calms their nervous systems and promotes improved healing.
My point is that all of our readings and discussions have given me confidence that I can use a similar approach with my clients with pain. I need to try to discover the cause of their pain. I need to stabilize the cause and make sure it is not dangerous. Once that is done, I need to help them grow and learn to break the vicious cycle they are likely battling through. The complex nervous system involvement in the dizzy world sounds extremely similar to the world of pain. Using words like "red light pain" and "green light pain" might help them learn to welcome certain types of pain as an opportunity to get stronger while other types of pain may indicate something needs to be adapted or changed. I need to teach them that the feeling like they could have pain is not the same as having pain.
-
Butera KA, Fox EJ, George SZ. Toward a Transformed Understanding: From Pain and Movement to Pain With Movement. Phys Ther. 2016 Oct;96(10):1503-1507. Butera_pain and movement_PTJ.pdf
-
Costigan M, Scholz J, Wolf CJ. Neuropathic Pain: A maladaptive response of the nervous system to damage. Annual Review Neuroscience, 2009;32:1-32. (not required; useful if this content is new to you) Costigan_Neuropathic pain_Annu Rev Neurosci.pdf
-
Bushnell CM, Ceko M, Low LA. Cognitive and emotional control of pain and its disruption in chronic pain. Nat Rev Neurosci 2013;14(7):502-511. Bushnell_emoational cognitive control pain_Nat Rev neurosci.pdf
-
Kerstman E, Ahn S, Battu S, Tariq S, Grabois M. Neuropathic Pain Handbook of Clinical Neurology 2013;110:176-87. (all should read this) Kerstman_Neuropathic pain.pdf
-
Pergolizzi J et al. Commentary: The development of chronic pain: physiological CHANGE necessitates a multidisciplinary approach to treatment. Current Medical Research & Opinion 2013;29(9):1127-1135. Pergolizzi_Chronic pain_CMRO.pdf


No comments:
Post a Comment